Currently, Preimplantation Genetic Screening (PGS) or Preimplantation Genetic Testing for Aneuploidies (PGT-A) are widely employed to select for embryos with normal chromosome number to implant in order to increase the implantation rates, lower miscarriage rates and also to avoid conceiving babies with chromosome abnormalities.
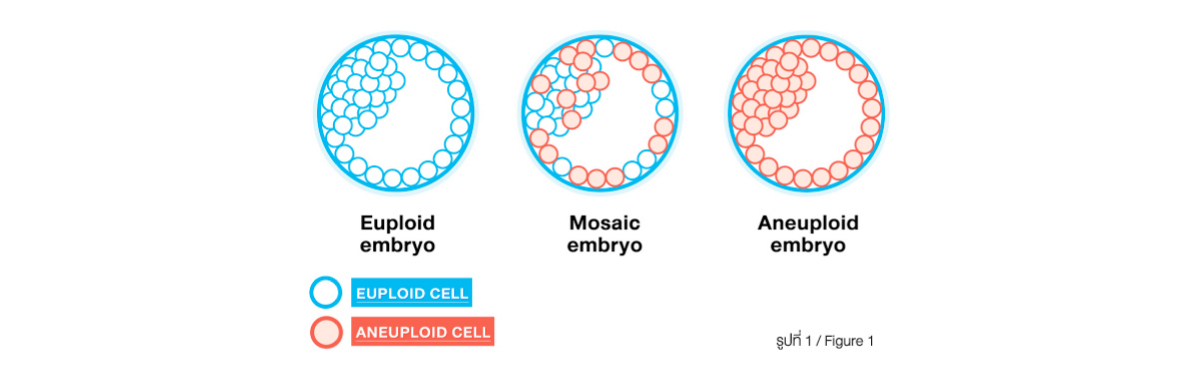
In general, people expect the PGS result of the embryos to be either having normal chromosome number (euploid) or having abnormal chromosome number (aneuploidy). In reality, there is another category of PGS result called “MOSAICISM” which has the presence of 2 or more population of cells, each with a different chromosome make-up within a single embryo (Figure 1). Approximately, 10-20% of embryos are expected to be mosaic.
Mosaicism has long been known in medicine. It has been studies for over 30 years on the presence of chromosome mosaicism in natural pregnancy. Prior studies have demonstrated the presence of the mixed-up of euploid and aneuploidy cells in placenta of the normal, healthy babies. The current embryo biopsy technique for PGS is to get trophectoderm biopsy in which trophectoderm is the part of embryos the eventually will develop into placenta of the pregnancy.
Normally, during cell division, the original cells with 23 pairs of chromosomes will double the number of chromatin before equally divided into 23 chromosomes for each daughter cells. In some circumstances, the chromatin division is unequal resulting in a cell line with extra copy of chromosome and another cell line with missing copy of chromosome (Figure 2)
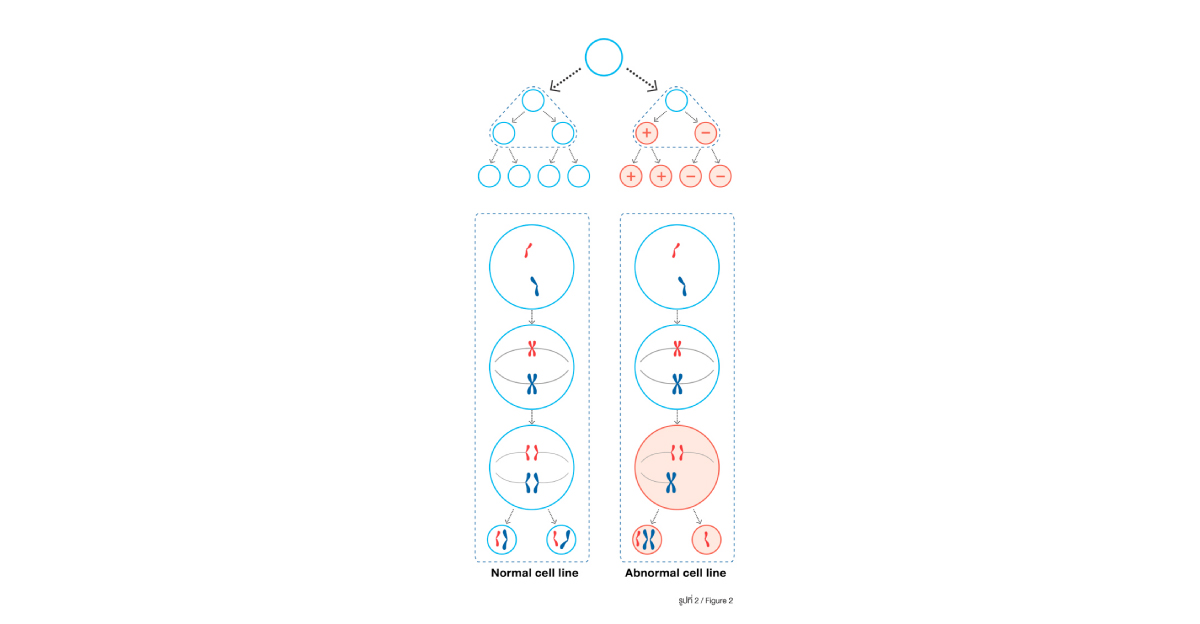
which leads to the occurrence of MOSAICISM. Though, it is demonstrated that 10-20% of embryos are mosaicism but the occurrence of mosaicism in live birth babies is not common. There are 2 main theories on the final development of mosaic embryos. The first theory believes that cells with normal chromosome (euploid) will continue to grow while cells with abnormal chromosome (aneuploidy) will end their development. This will convert mosaic embryos into normal embryos when the cells with abnormal chromosomes are finally eradicated. The other theory believes that cells with normal chromosome (euploid) will develop into the part of fetus/baby while cells with abnormal chromosome (aneuploidy) will mobilize into the part of placenta which will end up with pregnancy with normal fetus/baby but having mosaic placenta.
Occasionally, after obtaining PGS result, there is no embryo of normal chromosome to make use leaving patients with only embryos with abnormal chromosome and embryos with mosaicism. This will lead to the question on “What to do?”, “Should we use the embryos with mosaicism?”. Previously, many studies showed that PGS lower that chance of pregnancy for each treatment cycle partly due to embryo wastage by not using embryos which is labelled as “mosaic”. Result from many studies including Jetanin’s internal data show that transferring mosaic embryo can give implantation rates upto 40-50% without increasing the risk of fetal anomaly. Moreover, amniocentesis of pregnancy from the transfer of mosaic embryos mostly demonstrates normal chromosome of the fetus. Considering IVF practice in the old days when there was no suchtechnique to test for embryo chromosome status (PGS/PGT-A), these embryos of good quality will be used for transfer unknowing of their chromosome status. There was no increased risk of fetal chromosome abnormality from the transfer of embryos without knowing their chromosome status. From these information, it is reassuring of making use of mosaic embryos.
Currently, there are guidelines for transfer of mosaic embryos. It is recommended that in those undergo IVF/ICSI with PGS treatment for whom there is no euploid embryo for transfer, it is reasonable to have detailed discussion about the use of mosaic embryos for transfer. If the couples decide to have mosaic embryos transferred, they should be counselled about amniocentesis to confirm chromosome status of the fetus if it results in a viable pregnancy. Single embryo transfer should be employed to avoid multiple pregnancies so it is practical to terminate the pregnancy in the event of having viable pregnancy with abnormal chromosome. It is recommended to avoid transferring mosaic embryos which involve mosaicism of chromosome 13, 18, 21, X and Y as these may result in a viable pregnancy with fetal chromosome abnormalities. Also, it is not advisable to make use of embryos with mosaicism of multiple chromosomes.
For couples having “MOSAIC” embryos, it is advisable to discuss with your doctors on the condition of your embryos before making a decision to use or not to use those embyros.
Written by
Dr.Somjate Manipalviratn
Obstetrician and Gynecologist, Reproductive Medicine
Jetanin Hospital
JETANIN Journal Vol.10 No.3
